An Historical Perspective on SIJ Movement
Over the past 2 centuries, several theories describing form and function of the sacroiliac joint (SIJ) have been developed. The sacrum has been described as a keystone in an arch or, conversely, a hub suspended by ligaments. The sacrum has been thought to rotate around a transverse axis located through one of several different locations, including the center of the articular surface (Bonaire’s tubercle) [1] [2]p60-61 [3], several millimeters posterior to the articular surface [2]p62 [4] [5] [6], or approximately 5 to10 cm inferior to the sacral promontory [7] [8]. A current concept is that the sacrum does not rotate but rather slides linearly along a track between the iliac ridge and sacral groove [1] [9] [10]p49-51.
Weisl [1] noted that various authors, including Duncan 1854 and 1868, Wood 1859, Meyer 1878, Farabeuf 1894, Posth 1897/98, Latarjet 1928, Gray 1938, and Klein 1891 believed that the sacrum rotated about a horizontal axis centered at the syndesmosis (interosseous ligament) area of the sacroiliac joint, but he discounted that theory. Instead, his own investigation, and generally accepted one, is based on linear displacement, in which the sacrum appears to slide along the relatively straight lines of the iliac ridges in what is now known as nutation and counternutation. He found that the center of sacroiliac motion varied considerably within an individual, depending on body position and movement but, in general, existed 5 to10 cm below the sacral promontory. Lavignolle et al. [8], using more precise methods, had similar results and stated that the axis of motion in the sacroiliac joint is in the median sagittal plane near the symphysis pubis. However, because he thought that the sacrum’s movement actually consisted of straight line and angular movements, not rotary, Weisl said that the “concept of an ‘axis of rotation’ was meaningless in a rigid, mechanical sense”. Weisl’s work formed the basis for the linear, gliding movement pattern known today as nutation and counternutation. Wilder et al. [3], using surface topography techniques, reviewed the different axes of rotation proposed by Bonnaire, Farabeuf, and Weisl, and found a great deal of variation. They concluded that “The position of the axes of motion varies considerably between individual specimens.”
MOVEMENT PATTERNS
Kapandji [2]p64-67 described nutation as “anterior rotation of the sacrum about an axis constituted by the axial ligament…so that the promontory moves inferiorly and anteriorly while the apex of the sacrum and tip of the coccyx move posteriorly…Meanwhile the iliac bones are approximated whereas the ischial tuberosities move apart” (see Bilateral Nutation) Counternutation is the opposite. “The sacrum, pivoting around the axial ligament, rights itself so that the promontory moves superiorly and posteriorly and the apex of the sacrum and the tip of the coccyx move inferiorly and anteriorly.” In Unilateral Motion, we see the more common pattern of reciprocating side-to-side motion. When one side is in nutation, the other side is in counternutation. The terminology nutation pattern or counternutation pattern is used here to describe the continuation of nutation and counternutation occurring superior and inferior to the pelvis.
During nutation, the interosseous ligament winds and pulls the sacrum and ilium closer [11-13] [2]p64-65, but not together [3], so it is generally thought that nutation is more stable than counternutation. However, other than by a few authors [14]p143-209 [15];[16, 17] [18]p659-693 [19]p477-499, very little consideration is given to what happens when the sacroiliac joint hits the end point of range of motion in nutation and the ligaments cannot resist the force. The concept of the ligamento-muscular reflex [20-35] does not appear to have garnered enough recognition to significantly influence treatment regimens for the sacroiliac joint. One reason for this omission appears to be the popularity of the “keystone in an arch” concept of sacroiliac stability in which axial force is supposedly transmitted between the sacrum and ilium by direct contact of the two bones [9, 13]. However, realizing that the sacrum is suspended by ligaments [7, 36, 37], allows one to apply the view that, as in all other joints, ligaments function to provide a stopping point at the end of the range of motion and that excessive force produces tearing of the ligaments. As the joint space widens, the muscles activate or become inhibited, in order to reduce the distance between the joint surfaces [38, 39]. When excessive force sprains the ligaments that restrict sacroiliac nutation, nutation is no longer stable and the body reflexively moves toward counternutation.
GRAVITY’S EFFECT
Several researchers, influencing different disciplines, have pioneered the basic idea of gravity’s effect on nutation/counternutation, including Jungmann in osteopathy, DeJarnette in chiropractic, Janda in the medical field, and DonTigny in physical therapy. Because the gravitational line passes anterior to the sacral pivot (the axial sacroiliac joint) and posterior to the innominate pivot (the acetabulae), gravity results in anterior rotation of the sacrum and posterior rotation of the ilium (nutation) [2]p64-67 [1, 11] [40]p617 [41]p306 [42] (SEROLA PART 1). In this sense, nutation can be seen as the core movement of shock absorption. The winding of the interosseous ligament can be compared to that of a central spring in a watch, with a limited range of motion. The nutation muscles, assisted by gravity, wind the spring, and the counternutation muscles, assisted by the elasticity inherent in some ligaments and connective tissue, uncoil the spring. The entire musculoskeletal system participates in this cyclic movement.
Jungmann’s concept of gravitational strain pathology [16, 17], first introduced in 1928, recognized that the force of gravity, causing what we now describe as nutation, triggers many problems within the musculoskeletal system. He developed the pelvic index [19]p477, which is an objective radiographic measure of the distance between the sacral base and ilium in the direction of nutation, and found that it gradually increases throughout life as the musculoskeletal system loses its resistance to gravity. He termed this illness “gravitosis”, or “gravitational strain pathology” and attributed it to “chronic-progressive and degenerative conditions” in the low back, neck, shoulders, chest, abdomen, and legs. His concept was that many muscles contract to withstand the force of gravity and may become tight, and exhibit chronic fatigue and decreased strength. As a key part of treatment to this condition, he developed a device that encircles the pelvis like a belt with pads that contact mainly the sacral apex and symphysis pubis. This device places counter pressure on the lower sacrum and symphysis pubis, towards counternutation, working against the effects of gravity.
As a longtime researcher of Jungmann’s gravitational strain concept, Kuchera [18]p661 & 678 suggested that “Postural muscles and ligaments biomechanically resisting the force of gravity are subject to overuse and strain accompanied by pain.” He added, “Dysfunction and pain caused by gravity begin insidiously. It initiates pathophysiologic dysfunction, then disrupts homeostasis, and even results in structural change if it is not recognized and treated.”
In agreement with Jungmann, Kuchera [19]p480 listed muscles that respond to gravitational stress by either hyperactivity or inhibition. Hyperactive muscles included the “upper trapezius, levator scapulae, pectoralis major (upper part), pectoralis minor, cervical erector spinae, scalenus muscles, sternocleidomastoid, tensor fascia latae, hamstrings, hip adductors (short adductors), gastrocnemius/soleus, piriformis, and iliopsoas.” Inhibited muscles included the “latissimus dorsi, mid/lower trapezius, rhomboids, anterior cervical muscles, quadriceps, abdominals, and gluteus maximus.” He stated that “these general patterns are documented to be characteristic, and predictable (Institute for Gravitational Strain Pathology 1992, Janda 1986, Jungmann & McClure 1963, Kuchera 1995a, Travell & Simmons 1983, 1992).” In general, the Serola Theory agrees with Janda’s muscle grouping, with some exceptions.
DeJarnette [43] first described a similar lesion, and its correction, on the sacroiliac joint in 1969 [14, 43]p179 & 199, as part of a system of chiropractic diagnosis and treatment, called Sacral Occipital Technic.
DeJarnette defined Category II as “…a separation, strain or stress of the weight-bearing part of the sacroiliac (SI) joint.” He went on to say that the “…weight bearing part of sacroiliac joint slips and separates, tearing the interosseous fibers and cartilages, producing effusion of fluids into the joint space and producing primary area of inflammatory reactions.” He discussed the weight-bearing section (a syndesmosis) of the sacroiliac joint as affecting the entire musculoskeletal system, stating “The weight-bearing part of the sacroiliac joint is highly invested with proprioceptive fibers so the limbs may be oriented in space. When this articulation or joint separates from the sacrum, the excessive stress placed upon the ligaments which encapsulate this joint shout out an order for reflex muscle inhibition so as to regulate and control the reflex contraction of coordinating muscle groups.” Key involvement of the iliopsoas, trapezius, gluteus maximus, and hamstrings were noted, and that patients may experience chronic muscle tension with a Category 2 lesion. DeJarnette developed a method of treatment, using wedges, which is intended to re-align and compress the sacroiliac joint, remove effusion, balance proprioceptive input into the musculoskeletal system, and eliminate stress from the ligaments; this is the only method that allows the joint to heal.
Janda [44]p97 also found a pattern of contracted and inhibited muscles that is similar to those found independently in my own research and that of Jungmann. He stated that “Muscle imbalance develops mainly between muscles prone to develop tightness (triceps surae, hamstrings, one-joint thigh adductors, rectus femoris, iliopsoas, tensor fascia latae, piriformis, quadrates lumborum, erectors of the spine, pectoralis major and minor, upper trapezius and levator scapulae, sternocleidomastoideus, short deep neck extensors, flexors of the upper extremities) and muscles prone to develop inhibition (tibialis anterior; vasti, in particular, the medialis; the entire gluteal group, abdominal muscles [the obliques, however, are controversial]; lower stabilizers of the scapula; deep neck flexors [they tend to spasm, however, which is often misdiagnosed]; mainly the extensors of the upper extremities).” In another section, the role of many of these muscles will be discussed as they apply to the nutation lesion. In general, the Serola Theory agrees with Janda’s muscle grouping, with some exceptions.
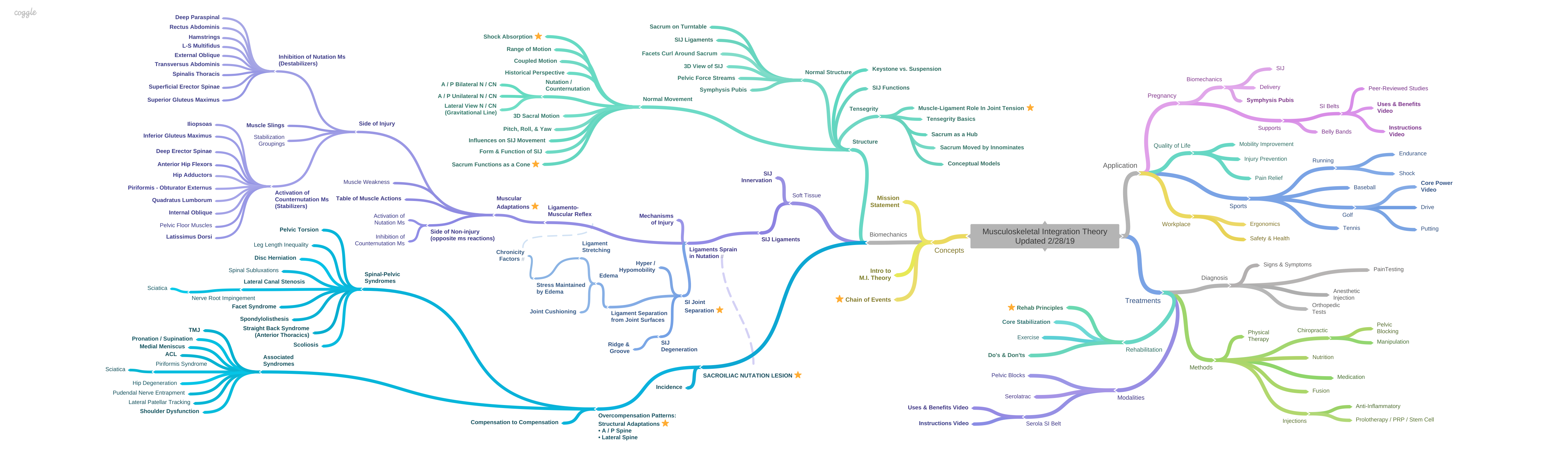
The difference between the works of Serola, Jungmann, and Janda is that, while Jungmann and Janda only give observations of the muscles’ actions, The Musculoskeletal Integration Theory gives the underlying cause, which leads to the muscles’ actions, with accompanying illustrations and videos, and is, therefore, more specific.
DonTigny [37, 45, 46] depicted a lesion that occurs in counternutation. He noted that, as one bends forward, the ilium rotates anteriorly, inferiorly, and laterally on the sacrum. In this position, the gravitational weight line shifts from posterior to the pivot points of the innominates, to their anterior. If the abdominal muscles are weak, the injury occurs “from an anterior rotation of the innominate bones on the sacrum” (counternutation). Although this appears to be possible, the patterns of muscular compensation most commonly observed [47] support nutation as the major lesion (see Muscular Adaptations). The difference is that the patient’s complaints result from the compensation to the injury, not the injury itself. Regardless of this interpretation, his basic concept agrees with the principles of nutation/counternutation. DonTigny advocates that, in the counternutation lesion, correction should be aimed at reversing the lesion, which may be seen to be promoting nutation.
On the other hand, the nutation lesion syndrome is based on the concept that counternutation is a compensating pattern, and correction is aimed at both reversing the compensating counternutation pattern and stabilizing the sacroiliac joint, so treatment may appear similar. But, the importance of stabilizing the sacroiliac joint cannot be overemphasized. Both concepts promote re-aligning the pelvis with gravity by rotating the ilium posteriorly. The major difference is that because DonTigny considers the injury to be a counternutation lesion, he may bring the structure toward nutation without considering the probability of going too far into nutation and overstressing the restraining ligaments. In contrast, correction of the nutation lesion stresses the importance of not aggravating the nutation ligaments by avoiding exercises that will put undue stress on the sacroiliac joint, either by holding the sacroiliac joint stable with a proper belt [48], or by use of a pressure gauge[49]p154.
References:
- Weisl, H., The movements of the sacroiliac joint. Acta Anatomica (Basel), 1955. 23(1): p. 80-91.
- Kapandji, I.A., The Physiology of the Joints. Vol. 3. 1977: Churchill Livingstone.
- Wilder, D.G., M.H. Pope, and J.W. Frymoyer, The functional topography of the sacroiliac joint. Spine, 1980. 5(6): p. 575-9.
- Bowen, V. and J.D. Cassidy, Macroscopic and microscopic anatomy of the sacroiliac joint from embryonic life until the eighth decade. Spine, 1981. 6(6): p. 620-8.
- Bakland, O. and J.H. Hansen, The “axial sacroiliac joint”. Anatomia Clinica, 1984. 6(1): p. 29-36.
- Bechtel, R., Physical characteristics of the axial interosseous ligament of the human sacroiliac joint. Spine J, 2001. 1(4): p. 255-9.
- Weisl, H., The ligaments of the sacroiliac joint examined with particular reference to their function. Acta Anatomica (Basel), 1954a. 20(3): p. 201-13.
- Lavignolle, B., et al., An approach to the functional anatomy of the sacroiliac joints in vivo. Anatomia Clinica, 1983. 5(3): p. 169-76.
- Snijders, C.J., Transfer of Lumbosacral Load to Iliac Bones and Legs: Part 1 – Biomechanics of Self-Bracing of the Sacroiliac Joints and its Significance for Treatment and Exercise. Clinical Biomechanics, 1993a. 8: p. 285-294.
- Lee, D., The Pelvic Girdle. 2nd ed. 1999: Churchill Livingstone.
- Weisl, H., The articular surfaces of the sacro-iliac joint and their relation to the movements of the sacrum. Acta Anatomica (Basel), 1954b. 22(1): p. 1-14.
- Solonen, K.A., The sacroiliac joint in the light of anatomical, roentgenological and clinical studies. Acta Orthopaedica Scandinavica. Supplementum, 1957. 27(Suppl 27): p. 1-127.
- Vleeming, A., et al., The role of the sacroiliac joints in coupling between spine, pelvis, legs and arms., in Movement, Stability, and Low Back Pain, A. Vleeming, et al., Editors. 1997, Churchill Livingstone. p. 53-71.
- DeJarnette, M., Sacral Occipital Technic Notes 1984. 1984: self published.
- Jungmann, M., Abdomino-pelvic pain caused by gravitational strain. Southwestern Medicine, 1961. 42(11): p. 501-508.
- Jungmann, M. and C.W. McClure, Backaches, Postural Decline, Aging, and Gravity-Strain. 1963, New York, NY: The Institute for Gravitational Strain Pathology, Inc.
- Jungmann, M., The Jungmann Concept of Gravitational Strain Pathology. An Introductory View. 1977, New York, NY: Institute for Graviational Strain Pathology.
- Kuchera, M.L. Diagnosis and Treatment of Gravitational Strain Pathophysiology: Research and Clinical Experience Correlates. Part II. in Second Interdisciplinary World Congress on Low Back Pain. 1995. San Diego, CA.
- Kuchera, M.L., Treatment of Graviational Strain Pathophysiology, in Movement, Stability, & Low Back Pain: The essential role of the pelvis, A. Vleeming, et al., Editors. 1997, Churchill Livinstone: New York. p. 477-99.
- Palmer, I., Pathophysiology of the medial ligament of the knee joint. Acta Chirurgica Scandinavica, 1958. 115(4): p. 312-8.
- Freeman, M.A. and B. Wyke, Articular reflexes at the ankle joint: an electromyographic study of normal and abnormal influences of ankle-joint mechanoreceptors upon reflex activity in the leg muscles. The British Journal of Surgery, 1967. 54(12): p. 990-1001.
- Ekholm, J., G. Eklund, and S. Skoglund, On the reflex effects from the knee joint of the cat. Acta Physiologica Scandinavica, 1960. 50: p. 167-74.
- Solomonow, M., et al., The synergistic action of the anterior cruciate ligament and thigh muscles in maintaining joint stability. The American Journal of Sports Medicine, 1987. 15(3): p. 207-13.
- Miyatsu, M., Y. Atsuta, and M. Watakabe, The physiology of mechanoreceptors in the anterior cruciate ligament. An experimental study in decerebrate-spinalised animals. The Journal of Bone and Joint Surgery. British volume, 1993. 75(4): p. 653-7.
- Kim, A.W., et al., Selective muscle activation following electrical stimulation of the collateral ligaments of the human knee joint. Archives of Physical Medicine and Rehabilitation, 1995. 76(8): p. 750-7.
- Guanche, C., et al., The synergistic action of the capsule and the shoulder muscles. The American Journal of Sports Medicine, 1995. 23(3): p. 301-6.
- Phillips, D., et al., Ligamentomuscular protective reflex in the elbow. The Journal of Hand Surgery. American volume., 1997. 22(3): p. 473-8.
- Petrie, S., et al., Mechanoreceptors in the palmar wrist ligaments. The Journal of Bone and Joint Surgery. British volume, 1997. 79(3): p. 494-6.
- Stubbs, M., et al., Ligamento-muscular protective reflex in the lumbar spine of the feline. J Electromyogr Kinesiol, 1998. 8(4): p. 197-204.
- Voigt, M., J. Jakobsen, and T. Sinkjaer, Non-noxious stimulation of the glenohumeral joint capsule elicits strong inhibition of active shoulder muscles in conscious human subjects. Neuroscience Letters, 1998. 254(2): p. 105-8.
- Indahl, A., et al., Electromyographic response of the porcine multifidus musculature after nerve stimulation. Spine, 1995. 20(24): p. 2652-8.
- Dyhre-Poulsen, P. and M.R. Krogsgaard, Muscular reflexes elicited by electrical stimulation of the anterior cruciate ligament in humans. Journal of Applied Physiology, 2000. 89(6): p. 2191-5.
- Sakamoto, N., et al., An electrophysiologic study of mechanoreceptors in the sacroiliac joint and adjacent tissues. Spine, 2001. 26(20): p. E468-71.
- Johansson, H., P. Sjolander, and P. Sojka, Actions on gamma-motoneurones elicited by electrical stimulation of joint afferent fibres in the hind limb of the cat. J Physiol, 1986. 375: p. 137-52.
- Tsuda, E., et al., Direct evidence of the anterior cruciate ligament-hamstring reflex arc in humans. The American journal of Sports Medicine, 2001. 29(1): p. 83-7.
Levin, S.M., The Sacrum in Three-Dimensional Space. Spine: State of the Art Reviews, 1995. 9(2): p. 381-88. - DonTigny, R.L., Mechanics and Treatment of the Sacroiliac Joint. J Manipulative Physiol Ther, 1993. 1: p. 3-12.
- Panjabi, M.M., The stabilizing system of the spine. Part II. Neutral zone and instability hypothesis. J Spinal Disord, 1992. 5(4): p. 390-6; discussion 397.
- Panjabi, M.M., The stabilizing system of the spine. Part I. Function, dysfunction, adaptation, and enhancement. J Spinal Disord, 1992. 5(4): p. 383-9; discussion 397.
- Oatis, C.A., Kinesiology. The Mechanics and Pathomechanics of Human Movement. 2004: Lippincott Williams & Wilkins.
- Neumann, D., Kinesiology of the Musculoskeletal System. Foundations for Physical Medicine. 2002: Mosby.
- DonTigny, R.L., Critical Analysis of the Functional Dynamics of the Sacroiliac Joints as They Pertain to Normal Gait. JOM, 2005. 27(1): p. 3-10.
- DeJarnette, M., Sacral Occipital Technic Notes 1969. 1969, Omaha: self published.
- Janda, V., Evaluation of Muscular Imbalance, in Rehabilitation of the Spine: A Practioner’s Manual, C. Liebenson, Editor. 1996, Williams & Wilkins. p. 97-112.
- DonTigny, R.L., Evalutation, manipulation, and management of the anterior dysfunction of the sacroiliac joint. The D.O., 1973. 14(1).
- DonTigny, R.L., Functional Biomechanics and Management of Pathomechanics of the Sacroiliac Joints. Spine: State of the Art Reviews, 1995. 9(2): p. 491-508.
- Vleeming, A., et al., Possible role of the long dorsal sacroiliac ligament in women with peripartum pelvic pain. Acta Obstet Gynecol Scand, 2002. 81(5): p. 430-6.
- Foley, B.S. and R.M. Buschbacher, Sacroiliac joint pain: anatomy, biomechanics, diagnosis, and treatment. Am J Phys Med Rehabil, 2006. 85(12): p. 997-1006.
- Richardson, C., et al., Therapeutic Exercise for Spinal Segmental Stabilization in Low Back Pain. 1999: Churchill Livingstone.