Ligamento-Muscular Reflex
The Ligamento-muscular response
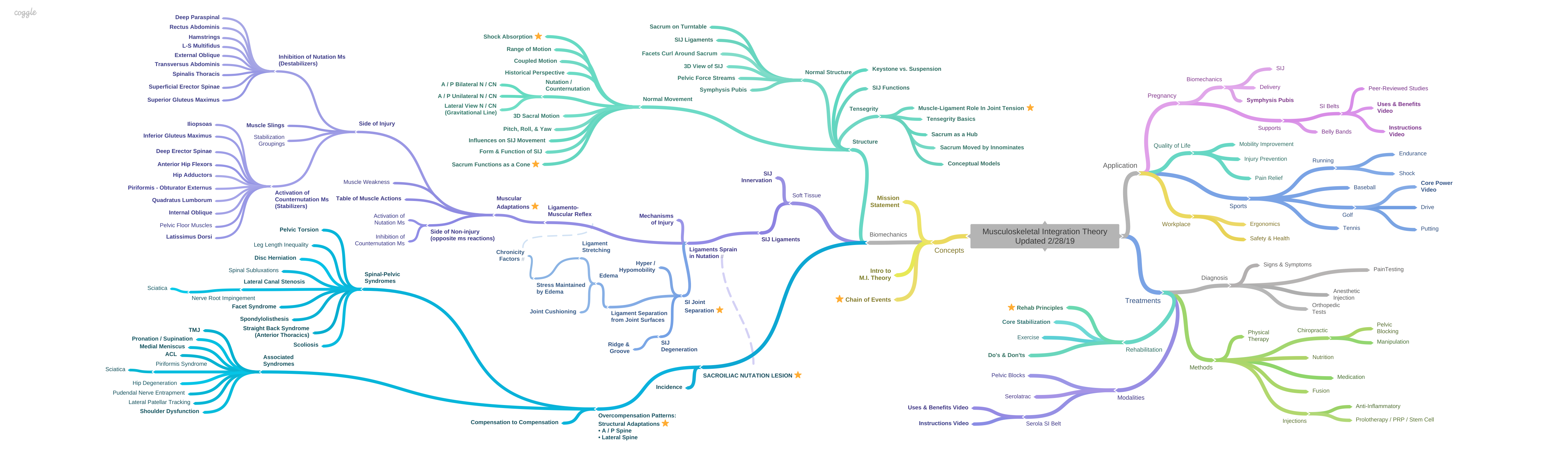
Ligaments are regulators of muscle tone. When a ligament is sprained, nerves within the ligament send signals to the muscles to stabilize excess movement by contracting some muscles and inhibiting others, in an attempt to remove the stress on the ligaments within the joints. The muscles that would stabilize the joint are activated and the muscles that would destabilize the joint are inhibited [1-4]. In other words, the ligaments are protecting themselves, and they use the muscles to do it.
For example, when the medial collateral ligament is sprained, the muscles on the medial side of the leg tighten to become secondary stabilizers. Their action would remove pressure from the medial collateral ligament by narrowing the space at the medial side of the leg. However, if the muscles on the lateral side of the leg contract, they would narrow the outside of the knee joint, which would, in turn, widen the medial side of the joint and stress the medial collateral ligament. As a result, the lateral muscles are inhibited [5].
With a sacroiliac joint injury, the counternutation muscles tighten and the nutation muscles slacken, in accordance with the agonist/antagonist relationship of muscles in all joints. Because the sacroiliac joint is at the center of motion and shock absorption, the effects are felt throughout the musculoskeletal system. The imbalance in these muscles leads to dysfunction, pain, and more injuries.
Today, in most musculoskeletal pain syndromes, treatment plans are aimed at treating the muscles, which are mainly reacting to protect the ligaments. But, stretching a tight muscle or strengthening an inhibited muscle may be counterproductive to joint stability (See Rehab Principles). https://www.serola.net/research-category/rehab-principles/
Appreciation of the ligamento-muscular reflex in our diagnosis and treatment regimens is lacking, yet it embodies one of the most important concepts in understanding and correcting musculoskeletal pain and dysfunction.
Ligament injuries may be the major cause of chronic back pain [6]. Neural receptors within injured ligaments can disrupt muscular response patterns and lead to spinal instability. The greater number of ligaments involved, the greater the muscular response, even at lower forces [7]. Considering that the sacroiliac joint is supported by a vast network of ligaments, it is reasonable to assume that a sprain of these ligaments will cause considerable muscular reaction. Eventually, poor balance and postural control may develop into abnormal posture, altered gait, and disturbed joint motion patterns throughout the structure.
Likewise, a lesion anywhere in the shock absorbing system may transfer additional stress to the sacroiliac joint and eventually lead to sacroiliac dysfunction. As a result, these and other shock absorbing mechanisms may become overloaded and may degenerate and fail [8].
History of the Ligamento-muscular Reflex
In 1900, Payr introduced the concept that ligaments are more than structural restraints; they provide a sensory feedback which activate or inhibit muscular action according to their effect on the damaged ligament. Payr [9] is credited [1, 5, 10] with introducing the concept that a ligament acts in a sensory capacity and can cause a muscular response to injury. He introduced the phrase “The Kinetic Chain” in which he says “Muscular hypertension is a manifestation of the reaction to joint injury of the active component of the Kinetic chain” (translated by Palmer).
In 1953, Andrew & Dodt [11, 12] were the first to make direct recordings from ligaments. They suggested that receptors in the ligaments are true position sensors and contribute proprioceptive input independent of the tone of the muscles.
In 1956, Cohen & Cohen [13] studied proprioceptors in uninjured ligaments in cats and found that flexing the knee activates the semitendinosus and inhibits the quadriceps; while extending the knee activates the quadriceps and inhibits the semitendinosus. Further, when the head was turned away from the tested leg, it would increase the flexion effect by inhibiting the quadriceps more than when the head was straight. To help describe this reaction, they coined the term “arthrokinetic reflex”, and described its function to “reinforce and coordinate flexion-extension movements of the leg.”
Soon afterward, in 1958, Palmer [5] conducted a study on an injured medial collateral ligament during movement. He wrote “…during movement an afferent flow emanates from the ligament, activating a muscular mechanism protecting the joint from subluxation to which it is vulnerable…Injury may lead to intensification of the afferent flow of the ligamentous protective reflex of such magnitude that a spastic contracture immobilizes the joint in semiflexion. If no treatment is administered, this spastic contracture may become fibrous and increasing atrophy results. If the semiflexed joint, of which both ligaments and muscles are unprotected, is exposed to weight bearing, repeated fresh violence will lead to irritative synovitis with further increased wasting and so on. Events are then caught up in a vicious cycle.” In this landmark paper, Palmer introduced the term “ligamento-muscular reflex.” Since then, this reflex has been identified in the knee [14-17], shoulder [1, 18-21], elbow [22], wrist [23], lumbar supraspinous ligament [7, 24], lumbar disc, facet joint and capsule [25, 26], ankle [27-30], TMJ [31], and sacroiliac joint [32-35], and more are being discovered regularly.
The ligamento-muscular reflex [5] agrees with the arthrokinetic reflex published two years earlier by Cohen & Cohen [13]. However, where the former dealt with responses from normal ligaments, Palmer specifically dealt with injured ligaments. He found that ligaments are proprioceptive, activating muscular adaptation patterns when they are sprained and stressed.
As time went on and the research became more sophisticated, there was a natural progression in the name of the reflex. In 1907, Sherrington [36] used the term “proprioception” to define a sense of posture, position, and movement. In 1956, Cohen and Cohen coined the “arthrokinetic reflex”. Two years later, Palmer identified a reflex as more specifically related to the ligament within the joint, hence “ligamento-muscular reflex”. Later, this reflex was further subdivided into: first, a protective mechanism that stimulated a monosynaptic reflex from the ligament to the skeletal motor neuron; and second, a polysynaptic reflex from the ligament, through multiple regulatory influences, to the gamma muscle spindle system.
Most of the research has been done on the latter system. With the ability to more closely identify the specific reflex by the neural response that it generates, the name “ligamento-muscular reflex” declined in use, yet it remains a generally descriptive term. In current literature, use of the vaguer, but more encompassing term, “proprioception” prevails. But it has been given an expanded meaning to include input from, and integration of, all types of receptors, including nociceptors and mechanoreceptors, within ligaments, tendons, muscles, fascia, skin, eyes, and other structures.
Until the 1980s, there had been a lot of controversy as to whether the ligamento-muscular reflex actually existed, and if so, whether it occurred through nociceptors or mechanoreceptors. Since then, many studies have not only confirmed its existence but have led to a general understanding of the interplay between ligament and muscle.
One early study had a major influence against the ligamento-muscular protective reflex. In 1959, Andersson & Stener [37], using myography, electromyography (EMG), and monosynaptic testing found no reflex effects from stretching the ligament. Later, discrepancies were discovered that explained their lack of results [15]. For example, the anesthetic used, ether, may have inhibited the reflex pathway. Also, the force used was far below what was needed to trigger the ligamento-muscular protective reflex. The required threshold for this monosynaptic reflex was just below the point of rupture.
In a later study, 1959, Petersen & Stener [38] demonstrated that the ligamento-muscular reflex occurred when the ligament was injured and the amount of stretch reached a significantly higher level than what was used by Andersson & Stener. The reflex was then abolished when the ligament was injected with an anesthetic; this caused the authors to conclude that the ligamento-muscular reflex occurred through pain receptors within the ligaments, and therefore was a nociceptive reflex rather than a mechanoreceptor reflex.
Investigating further, in 1962, Stener & Petersen [39] found strong contraction responses in the hamstrings and inhibition in the vastus medialis when the injured medial collateral ligament was stretched. They confirmed that the ligamento-muscular reflex in injured ligaments emanated from nociceptors, not mechanoreceptors, so a strong force was needed. They also noted that, when the supporting muscles were contracted prior to the ligament stress, it took considerably more force on the injured ligament to provoke a response than when the muscles were relaxed. This indicated that preparatory muscular contraction assisted in joint stability, and it formed a basis for understanding mechanoreceptor involvement through the gamma motor muscle spindle system.
In 1960, Ekholm, Eklund et al. [40] demonstrated that both increasing intra-articular pressure, and pinching of the joint capsule, caused inhibition in the knee flexors and contraction of the knee extensors. They also said that the method of preparing the cats by Andersson & Stener, above, provoked a strong extensor reflex that may have nullified the flexion reflex and led them to believe that the ligamento-muscular reflex did not exist. However, by properly spinalizing the cats, Ekholm, Eklund et al. were able to provoke a strong ligamento-muscular reflex. They also suggested that the reflex probably involved both mechanoreceptors and nociceptors.
In 1967, Freeman & Wyke [27] did an electromyographic study of normal and abnormal influences of ankle-joint mechanoreceptors from which they proposed that articular mechanoreceptors along with, to a lesser extent, cutaneous receptors, contribute to reflex coordination of muscle tone in posture and movement through the gamma motor muscle spindle system. They also proposed that these reflexes are modulated through higher centers in the brain stem, cerebellum, and cerebral cortex. Further, they suggested that these higher centers may contribute to persisting abnormalities in the postural reflexes, and tone, of muscles moving the affected joint. This work was important in changing the concepts of the ligament from a simple mechanical stabilizer to a sensory system able to regulate joint movement, tension, and stiffness, resulting in chronic imbalances.
In 1979, Pope [41] tested reflex timing in-vivo and found that the nociceptive system, and some mechanoreceptors, by acting quickly and directly on the motor neuron, can help to limit damage. On the other hand, he also found that the muscle spindle system will help in augmenting joint stability, after the initial injury, by increasing muscle stiffness in preparation for the next destabilizing event.
If the trauma is too sudden and forceful, neither system is sufficient to prevent joint injury.
Pope [41] analyzed the time it took for a skier to damage his knee in a fall, and found that the reflexes were too slow to prevent injury. However, others [15, 39, 42] suggested that Pope’s study disregarded the potential preparatory joint stiffness that may have existed at the time of injury, which would modify the response and may significantly lessen the degree of injury. In a normal joint, preparatory bracing may occur through visual or auditory cues but, in an injured joint, bracing will be maintained from the time of the initial injury.
Then, in 1980, Wyke [43], summarized the current literature, primarily from the previous 15 years of research in the Neurological Unit of the Royal College of Surgeons of England. He stated that nociceptors are part of a system that creates a pain response due to abnormal mechanical deformation (close to the point of ligament rupture) or chemical irritants, such as those encountered in inflammation. Nerves project from various tissues to specific areas of the cortex where the symptoms of pain may manifest. However, pain does not have to be evoked since other influences may inhibit or alter the pain sensation. An important concept is the final pathway that nociceptors take to the muscles – a monosynaptic reflex from the afferent nerve directly to the motor neuron ensures the fastest possible response. Nociceptors create a strong muscular reaction.
Some mechanoreceptors also act similarly, reacting to strong mechanical stimulation. But, instead of ascending to the cortex to be felt as pain, the stimulus is relayed to the gamma muscle spindle system to provide information for finer muscular control.
These mechanoreceptors influence the muscles through a complex set of neurons which incorporate input from several higher centers to provide a more measured response through the muscle spindle system. They help orient the body within space, and they feed information from the ligaments to the spindles within the muscles. The muscle spindles, in turn, regulate tone and contribute to joint stability. Because a number of synapses are involved, the response is relatively slow.
Through mechanoreceptors, ligaments provide both mechanical stability and sensory information. Position and movement senses are modulated through the gamma muscle spindle system, which provides this information to higher centers where they are modified. Then, together with input from ipsilateral and contralateral peripheral joints and skin, the descending signals are integrated in fusimotor neurons and relayed to the gamma spindle system within the muscle. The various inputs are finally integrated to control muscle stiffness and coordination, providing joint stability [44].
There are two types of response to ligament injury. To help limit immediate harm, the reaction may occur through a fast acting monosynaptic reflex directly from the afferent nerve to the motor neuron [5, 22, 43, 45].
Or, in an attempt to restore and maintain stability, and prepare the joint for future destabilizing events, a relatively slow acting polysynaptic reflex that is guided by input from higher centers to provide a more measured outcome, will activate the gamma muscle spindle system to induce muscles to produce joint stiffness [15, 27, 39, 44, 45], which may remain indefinitely [46] and play a role in altered firing patterns and coordination throughout the body [33].
Position and movement senses are modulated through the gamma muscle spindle system, which provides this information to higher centers, such as the brain stem, cerebellum, and cerebral cortex, where they are modified. Then, together with input from ipsilateral and contralateral peripheral joints and skin, the descending signals are integrated in fusimotor neurons and relayed back to the gamma spindle system within the muscle. The various inputs are finally integrated to control muscle stiffness and coordination, providing joint stability and preparing the joint for further damaging incidents [27, 44]. Because a number of synapses are involved, the response is relatively slow.
It was found that the response from an injured ligament varied markedly from that of a normal ligament, not in which muscles were affected, but in the degree of activation or inhibition. Neural responses from the ligaments lead to persistent muscle spasm and inhibition patterns resulting in altered joint function.
Panjabi [6] helped summarize the effects of ligament injuries on the structure by describing the spinal stabilizing system as consisting of three subsystems: spinal column, spinal muscles, and neuromuscular control unit. He points out research which suggests that, in addition to structural support, the spine functions as a transducer to coordinate muscle activity during motion. He stated that normal mechanoreceptors within ligaments and muscles generate transducer signals that measure vertebral position, movement, and load. This information is transferred back to the muscles to activate them in a defined sequence with respect to onset, activation level, and shut-off to provide smooth movement. His hypothesis is that injury corrupts the mechanoreceptors which then send corrupted transducer signals to the muscles resulting in corrupted muscle firing patterns and sequences. These corrupted messages would lead to undesirable changes. The word corrupted suggests the presence of errors that have been introduced unintentionally. However, the literature suggests otherwise. In an injured joint, research indicates that the muscles are activated in a definite pattern designed to protect the injured ligament. The muscles that would stabilize the joint are activated and the muscles that would destabilize the joint are inhibited [2-4, 14, 15, 21, 24, 32, 45].
Instead of corrupted signals from the receptors, I suggest that the signals are accurate and result in defined contraction/inhibition patterns which consistently alter the function and firing sequence of the muscles in order to protect the injured ligament.
Additionally, since nociceptors activate only after injury, close to the point of ligament rupture, it would appear that their function to perform after injury is according to design. If not for injury, they may not activate at all. Instead of corrupted signals from the receptors, I suggest that the signals are accurate and result in defined contraction/inhibition patterns which consistently alter the function and firing sequence of the muscles in order to protect the injured ligament. This protective function would be more consistent with Palmer’s suggestion that injury leads to intensification, rather than corruption, of afferent flow. At lower levels of injury, other mechanoreceptors also activate according to design through the gamma muscle spindle system.
In 1991, Johansson & Sojka[4] hypothesized two positive feedback loops that intensify and perpetuate muscle spasm in the affected muscle, and, in a chain reaction, spread to surrounding muscles, leading to increased joint stiffness.
In literature reviews, including 17 studies by Johansson and others, Johansson and Sjolander et al. [4] state that ligament injuries send altered sensory feedback to the muscle spindles. At certain thresholds, secondary muscle spindle afferents may project back to the muscle spindle, creating another positive feedback loop, “secondary spindle afferents – fusimotor neurons – muscle spindles”. This independent positive cycle greatly amplifies the effects of the aberrant input and may create persistently abnormal muscle stiffness and inhibition patterns which, in turn, may induce errors in muscular coordination and joint stability. Johansson [4]suggested that this “potentially vicious cycle” may be a significant part of chronic musculoskeletal pain syndromes and, in a chain reaction, spread to surrounding muscles, leading to increased joint stiffness. Importantly, the reflexes were significantly increased, generating a 79% larger muscle response, when loading was done during movement, emphasizing the enhanced susceptibility of ligaments to damage during strenuous activity [5, 15].
In addition, metabolites from muscle contraction may be augmented by ischemia to activate group III and IV muscle afferents, which stimulate gamma motor neurons and increase spindle sensitivity to stretch. In turn, the spindles increase the activation level of alpha motor neurons, causing increased reflex mediated stiffness in the primary muscle in a cycle of “increased metabolites – muscle stiffness – increased metabolites”. This vicious cycle may spread to surrounding muscles. “Such a distribution of the increased muscle stiffness to secondary muscles will further aggravate the vicious circle…[and] may constitute a mechanism or series of events by which several muscles, via positive feedback, will influence each other to increase the reflex mediated stiffness” [4].
Injured ligaments have also led to significantly slower reaction times in their associated muscles [15, 35, 47] and may be the cause of a joint suddenly giving out [48]. A delayed reaction time indicates altered proprioception. It follows that increased activity, such as sports or work involving bending, lifting, or twisting, increases susceptibility to further damage since the stress may be transferred to ligaments in other joints that may be unprepared to handle the load.
Stabilizing injured joints, especially the sacroiliac joint, due to its central role, should be a principal consideration in prevention and treatment of musculoskeletal injuries, and promoting fitness and well-being.
Application to Specific Joints
Ligamento-muscular reflexes have been found to occur in muscles that directly cross the joint, such as the knee or in muscles that do not directly cross the joint, as in the ankle [3, 30]. The muscular support of the sacroiliac joint is similar to that of the ankle in that no muscles go primarily across the joint. Instead, most movement occurs through a combination of muscles pulling the sacrum and innominates through various attachment points and vectors in a pattern of nutation and counternutation, with the axial joint as the pivot.
Most of the early literature was published on the medial collateral ligament of the knee, as described above. In the 1980’s, research started focusing on other ligaments and afferent nerves. Joints that have shown the presence of the ligamento-muscular reflex include the following:
Knee: In 1984, Stokes & Young [49] reviewed Young’s Eli Lilly Prize winning essay in which he defined “arthrogenous muscle weakness” as “weakness of muscles acting about an injured or inflamed joint. The weakness may be due to loss of muscle or inability to activate the muscle.” They discussed several possible causes for the inhibition including meniscectomy, peri-articular pathology, effusion, joint angle, ischemia, and pain. They presented evidence that validated the first four causes but discounted the last two causes.
Knee: In 1986, Johansson, Sjolander et al. [50], worked with electrical stimulation to the knees of cats. By stimulating the posterior articular nerve (PAN), they found excitatory and inhibitory effects, through the gamma motor neurons, to both flexor and extensor muscles on the same side, as well as the opposite side of the body. For the first time, effects on the gamma system were found to occur at low nerve thresholds. One important aspect of this investigation was that they found a very high response rate (greater than 93%) of both static and dynamic gamma cells to electrical stimulation of the afferent nerve. Their findings led them to suggest that their results, in addition to supporting Freeman and Wyke’ s hypothesis that the ligamento-muscular reflex, through the gamma muscle spindle system, contributes to “coordination of muscle tone and movement”, also suggested that this system may regulate joint stiffness and stability.
Knee: In 1987, Solomonow, Baratta et al. [45] studied the Anterior Cruciate Ligament (ACL) in both humans and cats. They were the first to show a relationship between sensory receptors in the ACL and EMG activity in the hamstrings. When the cat’s ligaments were loaded just below the point of rupture, a fast acting ligamento-muscular protective reflex arc was clearly established from the ACL to the hamstrings. In humans, in which loading to the point of rupture was not considered, a secondary, slower acting reflex was demonstrated, activating the hamstrings and inhibiting the quadriceps. They suggested that the muscle spindles moderated this slower response. Strengthening of the hamstrings was found to be of primary concern in rehabilitation, since their action supports the action of the ACL. Quadriceps strengthening was also demonstrated to help provide stability in well-conditioned athletes. But, it was suggested that the immediate goal is to strengthen the hamstrings, and then gradually increase the quadriceps strength.
Knee: In 1989, Sojka, Johansson et al. [51] and Johansson, Sjolander et al. [51] determined that a natural stimulation, such as stretching the posterior cruciate ligament in the knees of cats, exerts influence on the gamma muscle spindle system, rather than the beta fusimotor neurons. They found both inhibition and activation of muscles moving the knee joint. The effects were noticed at very low loads: 5 – 10 Newtons (100 N = 22.48 pounds), where it took 210 – 300 N to tear the ligament. They noted that the gamma motor neurons are influenced by low forces, whereas alpha motor neurons are influenced only by very high loads, close to that of ligament rupture [45]. Their findings strongly support the gamma muscle spindle system as the major mechanism controlling muscle tone and movement, as well as joint stiffness and stability, as noted by Freeman, Wyke, and Johansson, above.
Knee: In 1989, Brand [10] reviewed the existing literature and came to the conclusion that the ligaments provided little structural support during movement and that control is largely through joint geometry and muscular activity. He suggested that, with ligament injury, adaptive patterns occur over time, through both neural and muscular reprogramming. This can lead to recurrent problems, including joint instability, muscular spasm, apprehension upon certain movements, and giving way. When applied to the sacroiliac joint, and the large number of muscles involved, it is easy to understand the debilitation that can occur with a sacroiliac lesion. He also suggested, along with an increasing number of researchers, that surgical approaches should take into consideration the sensory role of ligaments. Rather than replace a ligament with an artificial structure, he suggested repair of the ligament, programs to increase proprioception, and encouragement of nerve in-growth. Fortunately, non-surgical repair of the sacroiliac ligaments is possible, but is, unfortunately, not well understood.
Knee: In 1990, Johansson, Lorentzon et al. [52] recorded the effects of increased tension on the cat ACL through the fusimotor effects on the gamma muscle spindle system. They found that the injured ligament evoked potent reflexes to the muscles through the gamma muscle spindle system, rather than through beta motor neurons. They found both excitatory and inhibitory effects on both static and dynamic fusimotor neurons. The low forces needed to evoke a reaction ruled out a nociceptive response. They stressed that, since the reflex effects on the muscles were markedly different in injured ligaments, it was very important to reconnect the torn ends of ligament. It was also important to establish a normal tension profile in the ligaments in order to provide correct proprioceptive input to muscles for proper joint stability. Since the “injured ligament is likely to cause a persistently disturbed sensory feedback from the joint”, rehabilitation programs should address the muscle imbalances as well as strength.
Knee: In 1994, Sojka, Sjolander et al. [53] and Sjolander, Djupsjobacka et al. [54] followed up with experiments on the medial and lateral collateral ligaments of the cat knee. They supported the theory that mechanoreceptors exert potent effects on the gamma muscle spindle system to provide reflex coordination in joint movement and stability, rather than on the motor neuron, as a means of a protective reflex against sudden trauma. Their work supported the concept that the gamma muscle spindle system is of primary importance in regulating muscle stiffness and joint stability.
Knee: In 1993, Miyatsu, Atsuta et al. [55], using decerebrate and spinalized cats to eliminate the effects of anesthesia, found that loading of the anterior cruciate ligament evoked muscular contraction in both the quadriceps and hamstrings through the posterior articular nerve. They stated that the ligamento-muscular reflex was elicited at relatively low load forces of 1% to 10% of the maximum tensile strength of the ligament. Their results suggested that the reflex from the ligament was due to mechanoreceptor influence through the gamma spindle system, in agreement with Freeman [27]and Johansson[56], above.
Knee: In 1993, Beard, Kyberd et al. [48] found that, in the knee with an injured ACL, the hamstrings reacted significantly slower to sudden perturbations than in a normal knee. Also, a direct relationship was shown to exist between slowed reaction time and the frequency of ‘giving out’, which indicated that this functional instability may be due to a loss of proprioception. They suggested that the delayed response time in reflex hamstring contraction can be used as an objective measure of proprioception in management of ACL deficiency.
Knee: Further, in 1994, Beard, Dodd et al. [57] divided patients into two groups. The control group performed traditional strengthening of the leg muscles, particularly the hamstrings, through open chain exercises. The experimental group performed closed chain exercises that were designed to improve proprioception by increasing hamstring reaction time. The experimental exercise program progressed by decreasing the stability of the starting position, increasing the number of repetitions, and finally, by removing visual feedback. Although there was no change in joint laxity in either group, the improvement in proprioception, and therefore function, was significantly greater in the experimental group.
Knee: In 1995, Kim, Rosen et al. [14] electrically stimulated the medial and lateral collateral ligaments and joint capsules in live subjects during valgus and varus stresses. They found that the muscles responded selectively to counter the stress applied to the ligament: the vastus medialis activated to counter the medial collateral ligament stress, and the vastus lateralis activated to counter the lateral collateral ligament stress. These results strongly supported a ligamento-muscular protective reflex in the human knee.
Knee: In 1996, Raunest, Sager et al. [15] found that loading the anteromedial fascicles of the ACL caused activation of the hamstrings and inhibition of the quadriceps. Loading the posterolateral fascicles of the ACL, or the anterior or posterior fascicles of the PCL, activated the quadriceps and inhibited the hamstrings, demonstrating that the muscular response was dependent on the directional stability of the ligament. Importantly, the reflexes were significantly increased, up to 79%, when loading was done during movement, emphasizing the susceptibility of ligaments to damage during strenuous activity. They found that pain receptors did not influence the results.
Knee: In 2000, Dyhre-Poulsen & Krogsgard [16], seeking results in vivo, inserted electrodes into normal ACL ligaments during arthroscopy. After surgery, when the effects of the anesthetic had worn off, they electrically stimulated the ACL. This study was important because, since isolating the ACL in live humans was unethical, knowing which tissue initiated the ligamento-muscular reflex was not possible. However, with this method, they proved that there is a clear link between the afferent nerve fibers in the ACL and changes in activity in the hamstrings and quadriceps. They stated that “…there are enough experimental data to confirm the existence of ‘ligamento-muscular reflexes’, probably through low-threshold mechanoreceptors that influence muscle activity via the gamma-muscle spindle system, whereas high threshold mechanoreceptors may exert effects directly onto the skeletomotorneurons.” Further, they state that “input from muscle and joint afferents converge with cutaneous input on the alpha-motorneurons”, suggesting multiple influences on the alpha motor neurons.
Knee: In 2005, Friemert, Faist et al. [47]found delayed latencies (time of response between ligament stress and activity in muscle) in people with ACL deficiencies. They said that the fact that the latencies were delayed demonstrated an indirect control of the reflex, possibly through the gamma motor neuron system, rather than a direct reflex from ligament to motor nerve.
Shoulder: In 1995, Knatt, Guanche et al.[18] stimulated a single branch of the musculoskeletal nerve terminating in that capsule and found that “The most important finding of this investigation is the fact that a reflex arc exists from the glenohumeral capsule to the biceps muscle, mediated by the musculocutaneous nerve and its articular branch…The presence of such reflex from the capsular ligaments confirms the evolving concept that the ligaments of a given joint function synergistically with the musculature crossing that joint to maintain its stability.”
Shoulder: Also in 1995, Guanche, Knatt et al. [19]electrically stimulated afferent nerves in the shoulder, demonstrating that a ligamento-muscular reflex arc exists between the mechanoreceptors in the capsule to the muscles crossing the joint. They stated “The existence of direct reflex arcs from the capsule to the musculature confirms and extends the concept that joint stability is not an exclusive or separate function of the ligaments and muscles but a synergistic affair between the ligaments and the associated muscles. The ligament-musculature synergism, which was first described in the knee joint, is now extended to the shoulder and most likely is present in other joints.”
Shoulder: In 1998, Voigt, Jakobsen et al. [20] inserted an electrode into the joint capsule of human subjects during surgery. After surgery, when the anesthetic had worn off, the joint was electrically stimulated. When only the anterior inferior part of the capsule, including the glenohumeral ligament, was stimulated, a strong inhibitory response was observed in voluntarily activated shoulder muscles, suggesting a potent ligamento-muscular reflex.
Shoulder: In 1996, Solomonow, Guanche et al. [1]inserted fine wire electrodes into the biceps, infraspinatus, supraspinatus, and acromiodeltoid muscles. By isolating and stimulating nerves from the capsular ligaments, they were able to evoke responses in the above muscles. They stated, “…the most important finding of this investigation is that a reflex arc mediated by articular branches of the subscapular and suprascapular nerves extends from mechanoreceptors in the glenohumeral capsule to several muscles crossing the joint. The presence of this reflex confirms the joint’s protective reflex concept suggested by Payr. This investigation shows that this synergism…probably exists in most other joints.”
Elbow: In 1997, Phillips, Petrie et al.[22]found a fast acting reflex in the medial collateral ligament of the cat elbow that elicited a contraction in the flexor-pronator muscles of the forearm and the flexor digitorum profundus of the wrist. Calculating speed of response, they noted that this could only be a monosynaptic protective ligamento-muscular reflex, acting from the articular afferent nerve directly onto the motor neuron.
Wrist: In 1997, Petrie, Collins et al.[23]found mechanoreceptors in the palmar ligaments of the wrist, including golgi organs, pacinian corpuscles, ruffini endings, and free nerve endings which led them to suggest that a ligamento-muscular reflex exists in the wrist.
Lumbar supraspinous ligament: In 1998, Stubbs, Harris et al.[24]established the presence of a ligamento-muscular reflex from the mechanoreceptors in the lumbar supraspinous ligament to adjacent paraspinal muscles. Although done with electrical stimulation, they found that the contracted muscles, by creating an extension response, relieved tension on the ligament that would be strained by flexion. They found the presence of types II and III mechanoreceptors. They suggested that type II (pacinian corpuscles) acted at low thresholds, monitored joint movement, and caused small adjustments in muscular activity for joint stability. Type III (golgi tendon-like endings) acted at high thresholds and created strong muscular responses to prevent injury and possible rupture, similar to the action of nociceptors, as described by Palmer[5], Peterson & Stener[38], Stener & Petersen, [39] and Ekholm & Eklund [40], above. This study also emphasized that the importance of ligaments in sensory feedback to the muscles in stability of the spine, and other joints, should be considered in surgery. Ligaments should not be cut and replaced with non-neural tissue but rather repaired, if needed, and/or supported to promote rebalancing of proprioceptive input.
Lumbar Supraspinous ligament: In 1998, Solomonow, Zhou et al.[7]mechanically deformed supraspinous ligaments in a cat at several levels and found that the strongest multifidus response occurred at the level of injury and one segment above and below. They also found that a single, isolated ligament withstood high forces before creating a muscular response. However, after observing that a group of ligaments were able to elicit a muscular response at much lower forces than a single ligament, they suggested that the combined action of all the ligaments around a joint elicited reflexive muscular activity at lower thresholds and contributed to greater stability at low to moderate loads. This is an important consideration when looking at the sacroiliac joint which has a very large number of ligaments and muscles which may be influenced by such a reaction.
Lumbar disc annulus facet joint and capsule: In 1995, Ihdahl, Kaigle et al. [25]found that electrical stimulation of the annulus and facet joint capsule provoked multifidus contractions that were significantly reduced with injection of lidocaine into the facet joint. They suggested that diseased or injured discs, or capsules, may cause reactive paraspinal muscular spasms as a protective reaction. Further, they suggested that such longstanding muscle spasms may induce ischemia in the muscles and result in back pain.
Lumbar annulus and zygapophyseal joints: In 1997, Indahl, Kaigle et al.[26]electrically stimulated nerves in the annulus and found contractions of the multifidus and longissimus muscles. The contractions were reduced by injection of physiological saline into the zygapophyseal joints. They stated that “The effect of the injection is most likely related to a stretch reflex from the capsule that excites inhibitory interneurons which in turn inhibit the motor neurons, thereby decreasing the muscle response.” They proposed that, in normal subjects, the injection may provoke pain but, in subjects with low back pain, the injection may relieve pain. This seemingly contradictory result may be explained by the idea that a stretch to normal zygapophyseal capsules will cause muscle spasm but stretch to the same capsule, in the presence of muscular spasm induced pain, secondary to annular disease, may inhibit the spasm and thereby reduce pain. They related this reaction to the well-known flexion-relaxation phenomenon, where back muscles become electrically silent in the fully flexed posture. They suggested that this silence is due to an inhibitory response on the muscles by the stretched zygapophyseal joint capsule. However, in patients with nucleus pulposus herniation, where the phenomenon was absent, they suggested that the injured discs may have provoked a strong enough muscular activation reflex to overcome the inhibitory stretch reflex from the capsules.
This study may explain how inhibitory muscular weakness may be somewhat overcome in well-trained athletes during activity, yet may still contribute to pain and weakness during periods of rest.
In 2000, Knutson [58] reviewing Johansson et al, above, stated that muscular induced stiffness, in turn, can result in reduced range-of-motion and increased sensitivity to pressure, which are characteristics of a subluxation type joint dysfunction. This complex will prevent stretching of the zygapophyseal joint capsules and the inhibitory reflex that they provoke. Knutson suggested that manipulation may stretch the capsules enough to elicit an inhibitory reflex on the paraspinal muscles and reset the gamma spindle system to break the perpetuating cycle of pain and muscle spasm.
Ankle: In 1967, Freeman & Wyke [27] investigated the effects of plantar and dorsi flexion on the gastrocnemius and tibialis anterior by electromyography. This study formed the basis of their conceptual link of the ligamento-muscular reflex, through articular mechanoreceptors, to the gamma motor neuron system. They also suggested that crushing pressure to a joint capsule can result in nociceptive input, and trigger muscular spasm directly through the alpha motor neuron.
Ankle: In 1994, Bullock-Saxton [28] tested the influence of vibration sensation in the ankle on EMG in leg and back muscles bilaterally, in both normal and injured subjects. She stated that “The significant delay in activation of the gluteus maximus muscle in the injured groups and the positive correlation between a poorer perception of vibration at 250 Hz and gluteal muscle activity suggests that joint injury involving sensory receptors could influence the function of muscles proximal and removed from the injury side.” Differences from normal were found in the gluteus maximus muscles on both sides. “This finding suggests that a reflex chain of events is not limited to the side of injury, but that there could also be implications for influences on the uninjured side.” She continued saying “Because muscles respond in different ways to peripheral injury, the results of this study suggest that the effects need to be sought in areas remote from the site of injury.”
Ankle: In 1999, Hintermann [29] reviewed the biomechanical aspects of the ankle ligaments. He found that radiological findings of ankle instability are highly unreliable. He stated that “The cause for chronic functional instability of the ankle joint is often not mechanical instability but impairment of ankle proprioception. A history of insecurity, instability, and giving way is far more important in diagnosis of ankle instability than the physical and radiographic examination.”
Ankle: In 2002, Solomonow & Lewis[30] stimulated the deltoid ligament of the ankle and, using EMG, observed contraction of the intrinsic foot muscles, including the quadratus, flexor digitorum brevis, abductor digiti minimi, and hallucis, which increased the arch of the foot and released tension on the deltoid ligament. They stated “…although the intrinsic muscles do not cross the ankle joint, they have a profound and direct impact on keeping this joint aligned and stable.” This study is important because it demonstrates that an injured ligament can cause contraction of muscles that don’t directly cross the joint but still act, through various vectors and levers, to stabilize an injured joint; this is an important point to consider when looking at the sacroiliac joint.
Sacroiliac Joint: In 1999, Indahl, Kaigle et al. [32]electrically stimulated the ventral portion of the sacroiliac joint and sacroiliac joint capsule in pigs. They found that stimulation of the ventral area of the sacroiliac joint primarily activated the gluteus medius and/or the gluteus maximus, and quadratus lumborum. Stimulation of the superficial dorsal layer of the joint capsule predominantly activated the multifidus muscles. This study established that the ligamento-muscular reflex existed between the sacroiliac joint and muscles that attach to the bones that make up the sacroiliac joint. They suggested that the sacroiliac joint was a regulator of pelvic and paraspinal muscles and, thereby, influences posture and lumbar segmental stability. Also, their finding that stimulating different areas of the sacroiliac joint activates different muscles indicates that structural compensation patterns may influence posture, and suggested that this reflex activation may lead to painful muscles over time. Further, the increased load during pregnancy may activate muscular patterns that lead to changes in walking, and other compensation patterns, due to stress on the mechanoreceptors within the sacroiliac joint ligaments.
Sacroiliac Joint: In 2002, Holm & Indahl [33], referring to the above study by Indahl, et al, placed EMG electrodes into the multifidus and longissimus muscles and then stimulated the annulus fibrosus. They stated that “Changes in loading on the sacroiliac joints may result in altered activation of the stabilizing muscles, and thus play an important regulatory function in stabilization and movement of the upper body during postural changes. Instability of a spinal motion segment…is believed to be manifested as a ‘slipping’ as a result of laxity in the motion segment. They suggested that “…this kind of hypermobility does not seem to occur but the motion pattern is greatly altered… and “may rather result in altered firing patterns and changes in the coordination pattern of the muscles.” They stated “Failure to adapt a functional muscle strategy to redistribute the increased loading may result in a dysfunction capable of generating pain.”
Sacroiliac Joint: In 2001, Sakamoto, Yamashita et al. [34] found mechanoreceptors in the sacroiliac joint, and suggested the presence of a ligamento-muscular reflex. They dissected the posterior sacroiliac ligaments and found that 97% of the mechanoreceptors were classified as nociceptors, indicating that the sacroiliac joint is a source of lower back pain.
Sacroiliac Joint: In 2006, Marshall & Murphy [35] demonstrated that delayed feed-forward activation in the transverse abdominis and internal oblique muscles was significantly improved by sacroiliac manipulation, signifying a definite relationship between the sacroiliac joint and muscular reflex timing patterns.
Reflex Inhibition Due to Effusion
In 1930, Sashin [59], studying cadavers, found that the sacroiliac joint is lined with a synovial membrane and, as such, contains a small amount of synovial fluid which is usually evidenced as moisture, which is all that is needed to lubricate the joint. He suggested that, in the intact joint, there is not much room for fluid because the space “is so narrow that the articulating surfaces appear to touch each other.” Too much separation would disturb the smooth tracking of the joint surfaces. Sashin also found that there is an increased amount of intra-articular fluid in the sacroiliac joints of women who died during pregnancy, or just after childbirth. He refers to other authors who found fluid in the sacroiliac joint space, including Meckel and Kollicker. DeJarnette [60], self-published, stated that the weight bearing part of the sacroiliac joint (the syndesmosis) is dry and without lubrication; however, “when this alignment of sacrum and ilium becomes misaligned, it also becomes moist due to seepage from the synovial or boot part of the sacroiliac articulation. When this happens, we have all the symptoms of infiltration with swelling and inflammation and pain.”
Some reference to the effects of effusion in other joints will help conceptualize what occurs with the sacroiliac joint nutation lesion.
Reflex sensory flow due to effusion was first shown in the knee, in 1953, by Andrew & Dodt [11]. They stated that “An increased intracapsular pressure was produced by injecting fluid into the synovial cavity. Simultaneous recordings of pressure and impulse traffic flow show that a raised pressure was a potent stimulus to slowly adapting endings in the capsule.” They did not say if the stimulus was excitatory or inhibitory.
Ekholm, Eklund et al.[40]followed up, in 1960, by increasing the inter-articular pressure of the knee joint of cats, by both increasing the volume of fluid within the joint and by pinching the joint capsule. They found that the knee extensors were inhibited while the flexors were facilitated. They stated that their results support Palmer’s concept of a ligamento-muscular reflex and that it can be initiated by capsular pressure.
In 1965, Deandrade & Grant [61] studied the effects of joint distension in humans by injecting their knee joints with plasma. They found that the increased pressure caused inhibition of the quadriceps muscles. They stated “The evidence suggests that distension of the knee may reflexly inhibit quadriceps contraction. Inhibition is associated with a feeling of heaviness and helplessness and can occur independent of pain sensibility. Increases in distended joints have been shown to occur many times daily….Reflex inhibition may lead to the muscle weakness, the atrophy, and the deformity that are seen in association with joint disease.” Injection of anesthetic delayed the inhibition until higher pressures were reached, which demonstrated that the inhibition was due to the effect of the internal pressure on the nerves. Disease of the nerves in that knee eliminated the inhibitory reflex completely.
In 1982, Kennedy, Alexander et al.[46]found that infusion of 60cc of normal saline caused a 30% to 50% inhibition of quadriceps contraction as demonstrated through the Hoffman reflex, which is similar to an electrically elicited deep tendon reflex. The inhibition was maintained as long as the effusion remained in the joint, which implies a long term inhibitory effect of internal joint pressure. The inhibition was eliminated with anesthesia. They suggested that ligament injury may lead to a destructive positive cycle, progressing to joint laxity, disrupted proprioceptive feedback, loss of muscular splinting, and repeated ligament injury. They also suggested that joint effusion may be a cause of the joint “giving way” at unpredictable times.
In 1988, Fahrer, Rentsch et al. [62] measured strength in the non-painful vastus medialis muscle of 13 patients with a Cybex II Dynamometer in addition to an EMG study. They found that “Our results were reproducible and demonstrated a mean increase of strength of 13.6% after aspiration of about 50 ml of fluid, with a further mean increase of 8% after intra-articular lignocaine injection…The fact that EMG activity also increased when there was a clear-cut gain in muscle strength after aspiration supports neurogenic rather than mechanical joint inhibition. Thus, our observations confirm and quantify the postulate of an inhibitory reflex mechanism blocking voluntary quadriceps innervation.”
In 1997, Indahl, Kaigle et al. [26] electrically stimulated a nerve in the annulus of the disc and elicited reflexes causing contraction of the lumbar multifidus and longissimus muscles. They then injected saline solution into zygapophyseal joints of lumbar vertebrae and found an inhibitory reaction to the involved muscles. They stated that “The effect of the injection is most likely related to a stretch reflex from the capsule that excites inhibitory interneurons which in turn inhibit the motor neurons, thereby decreasing the muscle response.”
Conclusion
A clear link has been established between injured ligaments and muscular response patterns. Muscles which support the injured ligaments are activated and muscles which would increase stress on the ligaments are inhibited. This spasm/inhibition complex develops through both fast-acting reflexes to help prevent further damage at the time of injury, as well as through slower acting reflexes to increase joint stiffness in preparation for the possibility of further trauma.
It is reasonable that sprained ligaments allow the sacroiliac joint surfaces to separate slightly. Fluid from the surrounding tissues, and from vessels within the syndesmosis, infiltrates the space between the sacrum and ilium, at the weight bearing syndesmosis, and furthers swelling, inflammation, and pain.
The increased pressure would stretch the interosseous and capsular ligaments. Nociceptors and mechanoreceptors within the ligaments respond by activating the ligamento-muscular reflex, which causes contraction of the muscles that remove stress from the ligament by attempting to pull the joint surfaces toward counternutation. At the same time, the reflex causes inhibition of the muscles that would promote nutation and further damage the ligaments.
An important point to consider is that the internal pressure of the swelling, pushing out on the joint surfaces, is countered by the external muscular compression; this is the body’s attempt to create stability. Considering that the interosseous ligament does not tear in the middle, but pulls away from the joint surfaces, the excess fluid within the joint may also prevent close enough approximation of the joint surfaces to allow for proper alignment and re-insertion of the interosseous ligament into the joint surfaces, thus prevent healing.
When the large complex of sacroiliac ligaments are considered in the context of the nutation lesion , it is likely that all muscles that promote a nutation pattern would be inhibited, while those that promote a counternutation pattern would be activated. This pattern can occur both locally and distant to the site of injury, including the opposite side of the body. An imbalance would exist between the nutation and counternutation muscles on one side of the body and also between the lesioned side and the normal or less lesioned side, causing postural distortions and altered function. Muscular performance and coordination could be reduced throughout the body.
Adaptive patterns occur over time, through both neural and muscular reprogramming, which can lead to recurrent problems, including joint instability, muscular spasm or inhibition, apprehension upon certain movements, feelings of heaviness and helplessness, and giving way.
Two positive feedback loops exist, which intensify and perpetuate muscle spasm in the affected muscles and, in a chain reaction, spread to surrounding muscles, leading to increased joint stiffness. Chronic stress can lead to continuously distorted muscle firing patterns which can alter joint angles and posture and generate pain in the back, hip, and upper legs. When applied to the sacroiliac joint, and the combined action of the large number of ligaments and muscles involved, it is easy to comprehend the debilitation that is possible with a sacroiliac lesion.
The SIJ is the center of the body, where the upper body (sacrum) meets the lower body (ilia). In order to absorb shock, the sacrum and ilia move in opposite directions. The nutation limiting ligaments are key central processing structures in handling and dispersing loads transferred throughout the body. The loads are processed and modifications are made to direct the muscles’ response. The large mass of ligaments at the sacroiliac joints are needed to withstand the stress of everyday load transfers; when they sprain, even microscopically, adaptations are made and the effects noted above are spread throughout the structure.
Mechanisms of injury for the sacroiliac joint occur throughout life, starting in childhood, such as falls, bending, lifting, and twisting, or chronic repetitive stress due to work or sports. It should be obvious that the sacroiliac joint is the central figure in most musculoskeletal injuries throughout the body. When the SIJ, as the core, becomes injured, ligaments cause muscular responses that torque the pelvis, and the body compensates by twisting the spine in a manner that affects the extremities. Further compensations are made such that ligaments in the spine and extremities become involved and spread the effects to specific muscles that help unload the local stress, whether it is in the foot, ankle, knee, hip, spine, shoulder, elbow, or cranium.
All responses circle back to the sacroiliac joint in a continuous loop to modify behavior and stabilize the entire system. As such, the sacroiliac joint having, by far, the largest mass of ligaments and, by far, the largest mass of muscles attaching directly to the bones composing the joint, directs the strongest regulating responses of any joint, and governs the rest of the musculoskeletal system. As you go through the Serola Theory, you will see the ligamento-muscular links connecting the entire musculoskeletal system into a functioning whole. From this perspective, it can be said that the sacroiliac joint is the precursor to most musculoskeletal injuries.
References:
- Solomonow, M., et al., Mechanoreceptors and reflex arc in the feline shoulder. Journal of shoulder and elbow surgery / American Shoulder and Elbow Surgeons … [et al.]. 1996. 5(2 Pt 1): p. 139-46.
- Solomonow, M. and M. Krogsgaard, Sensorimotor control of knee stability. A review. Scandinavian Journal of Medicine & Science in Sports, 2001. 11(2): p. 64-80.
- Solomonow, M., Ligaments: a source of work-related musculoskeletal disorders. Journal of Electromyography and Kinesiology, 2004. 14(1): p. 49-60.
- Johansson, H., Role of Knee Joint Ligaments in Proprioception and Regulation of Muscle Stiffness. Journal of Electromyography and Kinesiology, 1991. 1(3): p. 158-179.
- Palmer, I., Pathophysiology of the medial ligament of the knee joint. Acta Chirurgica Scandinavica, 1958. 115(4): p. 312-8.
- Panjabi, M.M., A hypothesis of chronic back pain: ligament subfailure injuries lead to muscle control dysfunction. European Spine Journal, 2006. 15(5): p. 668-76.
- Solomonow, M., et al., The ligamento-muscular stabilizing system of the spine. Spine, 1998. 23(23): p. 2552-62.
- Grieve, E.F., Mechanical dysfunction of the sacro-iliac joint. International Rehabilitation Medicine, 1983. 5(1): p. 46-52.
- Payr, E., Der heutige Stand der Gelenkchirurgie. Arch Klin Chir, 1900. 148: p. 404-51.
- Brand, R.A., A neurosensory hypothesis of ligament function. Medical Hypotheses, 1989. 29(4): p. 245-50.
- Andrew, B.L. and E. Dodt, The deployment of sensory nerve endings at the knee joint of the cat. Acta Physiologica Scandinavica, 1953. 28(4): p. 8287-96.
- Andrew, B.L., The sensory innervation of the medial ligament of the knee joint. J Physiol, 1954. 123(2): p. 241-50.
- Cohen, L.A. and M.L. Cohen, Arthrokinetic reflex of the knee. The American Journal of Physiology, 1956. 184(2): p. 433-7.
- Kim, A.W., et al., Selective muscle activation following electrical stimulation of the collateral ligaments of the human knee joint. Archives of Physical Medicine and Rehabilitation, 1995. 76(8): p. 750-7.
- Raunest, J., M. Sager, and E. Burgener, Proprioceptive mechanisms in the cruciate ligaments: an electromyographic study on reflex activity in the thigh muscles. The Journal of Trauma, 1996. 41(3): p. 488-93.
- Dyhre-Poulsen, P. and M.R. Krogsgaard, Muscular reflexes elicited by electrical stimulation of the anterior cruciate ligament in humans. Journal of Applied Physiology, 2000. 89(6): p. 2191-5.
- Friemert, B., et al., Differentiation of hamstring short latency versus medium latency responses after tibia translation. Experimental Brain Research. Experimentelle Hirnforschung, 2005. 160(1): p. 1-9.
- Knatt, T., et al., The glenohumeral-biceps reflex in the feline. Clinical Orthopaedics and Related Research, 1995(314): p. 247-52.
- Guanche, C., et al., The synergistic action of the capsule and the shoulder muscles. The American Journal of Sports Medicine, 1995. 23(3): p. 301-6.
- Voigt, M., J. Jakobsen, and T. Sinkjaer, Non-noxious stimulation of the glenohumeral joint capsule elicits strong inhibition of active shoulder muscles in conscious human subjects. Neuroscience Letters, 1998. 254(2): p. 105-8.
- Tsuda, E., et al., Direct evidence of the anterior cruciate ligament-hamstring reflex arc in humans. The American journal of Sports Medicine, 2001. 29(1): p. 83-7.
- Phillips, D., et al., Ligamentomuscular protective reflex in the elbow. The Journal of Hand Surgery. American volume., 1997. 22(3): p. 473-8.
- Petrie, S., et al., Mechanoreceptors in the palmar wrist ligaments. The Journal of Bone and Joint Surgery. British volume, 1997. 79(3): p. 494-6.
- Stubbs, M., et al., Ligamento-muscular protective reflex in the lumbar spine of the feline. J Electromyogr Kinesiol, 1998. 8(4): p. 197-204.
- Indahl, A., et al., Electromyographic response of the porcine multifidus musculature after nerve stimulation. Spine, 1995. 20(24): p. 2652-8.
- Indahl, A., et al., Interaction between the porcine lumbar intervertebral disc, zygapophysial joints, and paraspinal muscles. Spine, 1997. 22(24): p. 2834-40.
- Freeman, M.A. and B. Wyke, Articular reflexes at the ankle joint: an electromyographic study of normal and abnormal influences of ankle-joint mechanoreceptors upon reflex activity in the leg muscles. The British Journal of Surgery, 1967. 54(12): p. 990-1001.
- Bullock-Saxton, J.E., Local sensation changes and altered hip muscle function following severe ankle sprain. Physical Therapy, 1994. 74(1): p. 17-28; discussion 28-31.
- Hintermann, B., Biomechanics of the unstable ankle joint and clinical implications. Medicine and Science in Sports and Exercise, 1999. 31(7 Suppl): p. S459-69.
- Solomonow, M. and J. Lewis, Reflex from the ankle ligaments of the feline. Journal of Electromyography and Kinesiology, 2002. 12(3): p. 193-8.
- Clark, R.K. and B.D. Wyke, Temporomandibular arthrokinetic reflex control of the mandibular musculature. The British Journal of Oral Surgery, 1975. 13(2): p. 196-202.
- Indahl, A., et al., Sacroiliac joint involvement in activation of the porcine spinal and gluteal musculature. Journal of Spinal Disorders, 1999. 12(4): p. 325-30.
- Holm, S., A. Indahl, and M. Solomonow, Sensorimotor control of the spine. Journal of Electromyography Kinesiology, 2002. 12(3): p. 219-34.
- Sakamoto, N., et al., An electrophysiologic study of mechanoreceptors in the sacroiliac joint and adjacent tissues. Spine, 2001. 26(20): p. E468-71.
- Marshall, P. and B. Murphy, The effect of sacroiliac joint manipulation on feed-forward activation times of the deep abdominal musculature. Journal of Manipulative and Physiological Therapeutics, 2006. 29(3): p. 196-202.
- Janda, V., Sensory Motor Stimulation, in Rehabilitation of the Spine: A Practioner’s Manual, C. Liebenson, Editor. 1996, Williams & Wilkins. p. 319-328.
- Andersson, S. and B. Stener, Experimental evaluation of the hypothesis of ligamento-muscular protective reflexes. II. A study in cat using the medial collateral ligament of the knee joint. Acta Physiol Scand, 1959. 48(Suppl 166): p. 27-49.
- Petersen, I. and B. Stener, Experimental evaluation of the hypothesis of ligamento-muscular protective reflexes. III. A study in man using the medial collateral ligament of the knee joint. Acta Physiol Scand, 1959. 48(Suppl 166): p. 51-61.
- Stener, B. and I. Petersen, Electromyographic Investigation of Reflex Effects Upon Stretching the Partially Ruptured Medial Collateral Ligament of the Knee Joint. Acta Chirurgica Scandinavica, 1962. 124.
- Ekholm, J., G. Eklund, and S. Skoglund, On the reflex effects from the knee joint of the cat. Acta Physiologica Scandinavica, 1960. 50: p. 167-74.
- Pope, M.H., et al., The role of the musculature in injuries to the medial collateral ligament. J Bone Joint Surg Am, 1979. 61(3): p. 398-402.
- Johansson, H., P. Sjolander, and P. Sojka, Receptors in the knee joint ligaments and their role in the biomechanics of the joint. Crit Rev Biomed Eng, 1991. 18(5): p. 341-68.
- Wyke, B., Receptor systems in lumbosacral tissues in relation to the production of low back pain. The Lumbar Spine and Back Pain, 1980: p. 97-107.
- Johansson, H., P. Sjolander, and P. Sojka, A sensory role for the cruciate ligaments. Clin Orthop Relat Res, 1991(268): p. 161-78.
- Solomonow, M., et al., The synergistic action of the anterior cruciate ligament and thigh muscles in maintaining joint stability. The American Journal of Sports Medicine, 1987. 15(3): p. 207-13.
- Kennedy, J.C., I.J. Alexander, and K.C. Hayes, Nerve supply of the human knee and its functional importance. The American Journal of Sports Medicine, 1982. 10(6): p. 329-35.
- Friemert, B., et al., Intraoperative direct mechanical stimulation of the anterior cruciate ligament elicits short- and medium-latency hamstring reflexes. Journal of Neurophysiology, 2005. 94(6): p. 3996-4001.
- Beard, D.J., et al., Proprioception after rupture of the anterior cruciate ligament. An objective indication of the need for surgery? J Bone Joint Surg Br, 1993. 75(2): p. 311-5.
- Stokes, M. and A. Young, The contribution of reflex inhibition to arthrogenous muscle weakness. Clinical Science (London, England: 1979), 1984. 67(1): p. 7-14.
- Appelberg, B., H. Johansson, and P. Sojka, Fusimotor reflexes in triceps surae muscle elicited by stretch of muscles in the contralateral hind limb of the cat. J Physiol, 1986. 373: p. 419-41.
- Sojka, P., et al., Fusimotor neurones can be reflexly influenced by activity in receptor afferents from the posterior cruciate ligament. Brain Res, 1989. 483(1): p. 177-83.
- Johansson, H., et al., The Anterior Cruciate Ligament. Neuro-Orthopedics, 1990. 9: p. 1-23.
- Sojka, P., et al., Influence from stretch-sensitive receptors in the collateral ligaments of the knee joint on the gamma-muscle-spindle systems of flexor and extensor muscles. Neurosci Res, 1991. 11(1): p. 55-62.
- Sjolander, P., et al., Can Receptors in the Collateral Ligaments Contribute to Knee Joint Stability and Proprioception via Effects on the Fusimotor-Muscle Spindle System? An experimental study in the cat. Neuro-Orthopedics, 1994. 15: p. 65-80.
- Miyatsu, M., Y. Atsuta, and M. Watakabe, The physiology of mechanoreceptors in the anterior cruciate ligament. An experimental study in decerebrate-spinalised animals. The Journal of Bone and Joint Surgery. British volume, 1993. 75(4): p. 653-7.
- Johansson, H., P. Sjolander, and P. Sojka, Actions on gamma-motoneurones elicited by electrical stimulation of joint afferent fibres in the hind limb of the cat. J Physiol, 1986. 375: p. 137-52.
- Beard, D.J., et al., Proprioception enhancement for anterior cruciate ligament deficiency. A prospective randomised trial of two physiotherapy regimes. J Bone Joint Surg Br, 1994. 76(4): p. 654-9.
- Knutson, G.A., The role of the gamma-motor system in increasing muscle tone and muscle pain syndromes: a review of the Johansson/Sojka hypothesis. J Manipulative Physiol Ther, 2000. 23(8): p. 564-72.
- Sashin, D., A critical analysis of the anatomy and the pathologic changes of the sacro-iliac joints. The Journal of Bone and Joint Surgery, 1930. 12: p. 891.
- DeJarnette, M., Sacral Occipital Technic Notes 1984. 1984: self published.
- Deandrade, J.R., C. Grant, and A.S. Dixon, Joint Distension and Reflex Muscle Inhibition in the Knee. The Journal of Bone and Joint Surgery. American volume, 1965. 47: p. 313-22.
- Fahrer, H., et al., Knee effusion and reflex inhibition of the quadriceps. A bar to effective retraining. The Journal of Bone and Joint Surgery, 1988. 70(4): p. 635-8.